

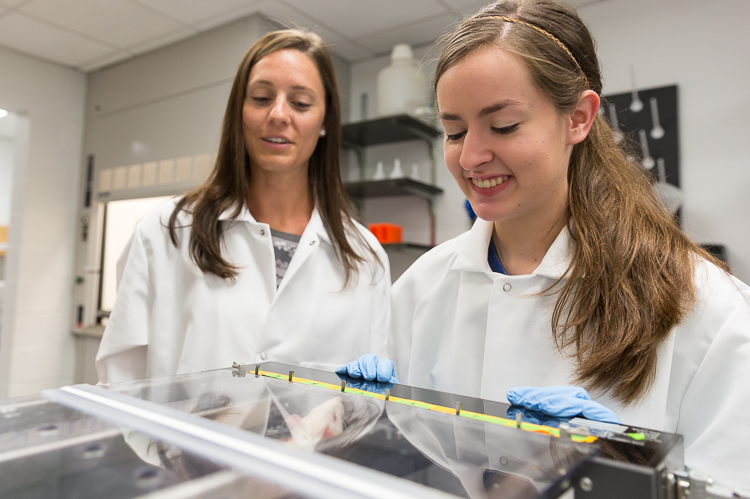
It’s a rainy Friday, and Health Sciences Prof. Emily Besecker and Theresa Blickenstaff ’20 are back in the Science Center after braving the elements to grab a celebratory lunch in town. It’s Blickenstaff’s last official day of working in Besecker’s lab for the summer. “We’ll know the results of the first part of our experiment by tonight,” says Besecker, looking sideways at Blickenstaff. “We debated waiting.” In science, there’s always the risk that your results will completely contradict your hypothesis. Besecker gestures behind her to dark storm clouds rolling across the sky. “Hopefully this isn’t some kind of omen.”
Besecker and Blickenstaff have been working on a project to determine the effects of treadmill training on solid meal gastric emptying—or, translated, the impact of exercise on the function of the gastrointestinal tract. It seems like a tangential topic for Besecker, whose work primarily focuses on spinal cord injuries. But there is a connection. Following spinal cord injuries, many people experience a loss of function in the gastrointestinal tract. Besecker said a growing number of studies indicate the vagus nerve—the longest nerve of the autonomic nervous system, which is involved in the control of organs like the heart, lungs, and digestive tract—could be involved in this loss of function. Strangely, the vagus nerve isn’t damaged in a spinal cord injury. This anomaly isn’t well understood by scientists, but Besecker and Blickenstaff hypothesize that exercise may be a treatment for gastrointestinal issues. Indirectly, this could provide clues for their root cause in the spinal cord injury population.
Besecker said there are currently over 280,000 people with spinal cord injuries in the U.S., and 17,000 new spinal cord injuries occurring each year. According to a survey by a leading researcher in the field, of all the functions they lost, people with spinal cord injuries ranked regaining visceral functions, like control of their bladder, bowel, and sexual function, at the top of the list—above regaining the ability to walk. Because spinal cord injuries result in the loss of sensation, daily things we take for granted, like feeling the urge to urinate, are lost. This can become life threatening. “If your bladder is full, it becomes a noxious stimulus, increasing heart rate, blood pressure, and the outcome could be a stroke. Regaining control over these functions is important for their quality of life, and life itself,” says Besecker.
Besecker is interested in better understanding how the stomach is controlled by the autonomic nervous system. “We know there are gastrointestinal deficits in the spinal cord injured population, but it’s poorly understood why these deficits are occurring—so we’re trying to get a better understanding of the circuitry involved and to improve the signaling through exercise.”
Besecker and Blickenstaff use two measures to analyze the impact of exercise on the gastrointestinal tract. The first is the rate of gastric emptying, or how quickly food leaves the stomach. Their hope, Blickenstaff says, is the data, which they are still analyzing (not because it was raining and they were superstitious, but because the results took longer than anticipated to analyze), will show that the rate of gastric emptying is higher in a test group given the treatment of exercise, and lower in the sedentary control group.
To collect the data, Blickenstaff has been a personal trainer of sorts this summer, motivating a team of male rats to run on a treadmill. The rats ran 5 days each week for 8 weeks at a moderate speed, taking breathalyzer tests throughout the summer—once at the beginning, again in the middle, and finally at the end of the experiment—to measure how much of the stable isotope (aka a piece of pancake) they metabolize.
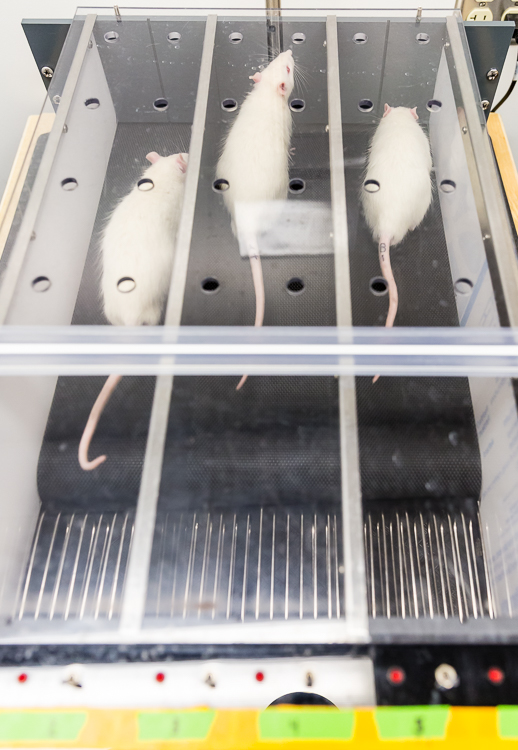 “My job is to keep [the rats] on the treadmill,” Blickenstaff says. “We started with using brushes to prod them, but they got used to it and it was no longer effective, so we switched to cardboard paddles to move them forward. But they got stressed out by that.” Stress is bad because it could impact the gastric emptying and throw another variable into the mix. So three weeks ago, she started using bursts of air. The rats are allowed to rest, but the exercise is meant to mimic a regular session of exercise that you’d expect a human to complete. “Our goal is to be able to say they spent at least 75% of the time they’re supposed to be on the treadmill on the treadmill. It’s been a day-to-day thing—one day something works, and one day it doesn’t.”
“My job is to keep [the rats] on the treadmill,” Blickenstaff says. “We started with using brushes to prod them, but they got used to it and it was no longer effective, so we switched to cardboard paddles to move them forward. But they got stressed out by that.” Stress is bad because it could impact the gastric emptying and throw another variable into the mix. So three weeks ago, she started using bursts of air. The rats are allowed to rest, but the exercise is meant to mimic a regular session of exercise that you’d expect a human to complete. “Our goal is to be able to say they spent at least 75% of the time they’re supposed to be on the treadmill on the treadmill. It’s been a day-to-day thing—one day something works, and one day it doesn’t.”
The second measure they’re interested in is neuronal changes, which they’ll analyze this fall. They inject a colored dye into the rats’ stomach that travels the length of the vagus nerve and highlights the neurons responsible for sensing what’s happening in the stomach. With the dye-filled neurons, they will use various assays to see if there is a neuronal difference between the treatment and control groups. Their hypothesis is that the morphology of the sensory neurons innervating the stomach will change in the rats that exercise.
“Thinking of the nervous system like a circuit,” Besecker says, “input drives output. So any time you’re putting more in, you expect to get more out. So we’re hoping to show exercise increases that sensory signal, which drives greater motor output, causing the stomach to function better through increased gastric emptying.” In the spinal cord injury population, gastric emptying is delayed. “If we see that we are able to increase the sensory signal to drive better output, that would significantly help the spinal cord population with gastric emptying.” Some studies have shown that these effects don’t become apparent immediately, so there is a need for longer term research.
Blickenstaff said having the opportunity to continue working with Besecker beyond the summer appealed to her. She is interested in pursuing medical school, so she sees this research—grounded deeply in principles of anatomy and physiology—as an opportunity to learn how research directly impacts helping people while honing her skills.
In a project such as this, it’s not uncommon for offshoots of ideas to present themselves, and often students are able to adopt complementary independent projects over several years. Soft-spoken and thoughtful, Blickenstaff is just entering her sophomore year, but she’s already hooked on the process of conducting research. (In part, because of the Introduction to Phage Biology course, which provides first-year students with immediate hands-on classroom research experience.) “I want to learn all the skills that I need to be eventually more independent in working and conducting research, starting from where I am now and working my way up,” she says. “It’s been valuable experiencing the beginning stages of a study and [seeing it through to] completion.”
When she started working in Besecker’s lab, Blickenstaff helped write a grant for research funding from the College, oversaw the delivery of the rats, and helped the rats acclimate to their new environment. “That kind of work helped me to see where we are and what our starting point is,” she says. “Dr. Besecker really involved me. I am grateful to do this research coming off freshman year. Not having taken college-level anatomy classes, I was still allowed to do this and learn from the experience. I’ve had a lot of fun—it’s been a summer of science.”
“That’s been the goal from day one,” agrees Besecker. “I want students to feel as much a part of the research as possible, to make it feel like a collaborative effort. It’s our lab now. We are a research team, answering questions we both find of interest.”
This summer, 61 students, including Blickenstaff, received support from the Cross-Disciplinary Science Institute (X-SIG) to complete science research. The program also provides funding for professional development for faculty.


